What do you know about calcium?
Most people know that calcium is important for healthy bones, that it is found in dairy and, for the most part, it doesn’t seem like a very interesting nutrient. As such, it doesn’t get paid much attention.
Therefore, it’s not surprising to learn that most of us don’t get enough calcium in our diet (1). What’s interesting is that this is the case even though there is generally a good supply of dairy foods and other calcium-rich foods in Australia.
This article will cover why calcium is important for your health, who is at risk of the effects of low calcium, and how you can get enough calcium in your diet.
Why do I need calcium?
Calcium is a mineral which is essential for the growth and maintenance of the skeleton. It gives strength and structure to bones and teeth.
Calcium is also important for the functioning of muscles, cardiovascular and nervous systems.
Why is it a problem if I don’t get enough?
During digestion, the calcium in food is absorbed through the small intestine into the bloodstream. From there, it is used for many functions across the body, or stored in the bones.
If there is not enough calcium in the diet, the body takes calcium from the bones so that it can perform its important functions. Over time, this can lead to osteopenia or osteoporosis, where the bones become weak and can fracture easily. The signs of osteoporosis are not obvious, and it may not be diagnosed until a fracture occurs. Although it is generally a preventable condition, it is estimated that 20% of people aged 75 years and above have osteoporosis (2).
When it comes to your long-term health and wellbeing, it is much better to prevent a fracture than to recover from one!
To do so, it is especially important to get enough calcium before the age of 30, as this is when peak bone mass is achieved. After this time, more bone mass is lost than is formed, and bone mineral density decreases.
Although calcium might be included in your blood test results, this does not indicate bone mass status. This is because the blood test measures calcium in your blood and most of your body’s calcium is stored in your bones. Instead, a bone mineral density scan can indicate how healthy your bones are.
Who is at risk?
Some key groups who may be at risk of a low calcium intake or low bone mineral density are:
- People who have removed dairy from their diet.
- People with coeliac disease or other conditions that may affect the absorption of calcium.
- People with increased calcium needs (e.g. children & adolescents have high needs due to growth, and older adults have increased requirements due to increased bone losses with ageing).
- People with low Vitamin D, which is important for the absorption of calcium.
- People with RED-S (Relative Energy Deficiency in Sport) (3).
Other risk factors include: ageing, sex (osteoporosis is more common in females), family history of the condition, low body weight, smoking, excess alcohol consumption, physical inactivity, long-term corticosteroid use and reduced oestrogen level (2).
How much do I need?
Below are the recommended daily intakes (RDI) for calcium, developed by the National Health and Medical Research Council (NHMRC) (4):
| Recommended Daily Intake (RDI) | |
| Children | |
| 0-6 months | 210mg |
| 7-12 months | 270mg |
| 1-3 years | 500mg |
| 4-8 years | 700mg |
| 9-11 years | 1000mg |
| 12-18 years | 1300mg |
| Adults | |
| Men 19-70 years | 1000mg |
| Men >70 years | 1300mg |
| Women 19-50 years | 1000mg |
| Women >50 years | 1300mg |
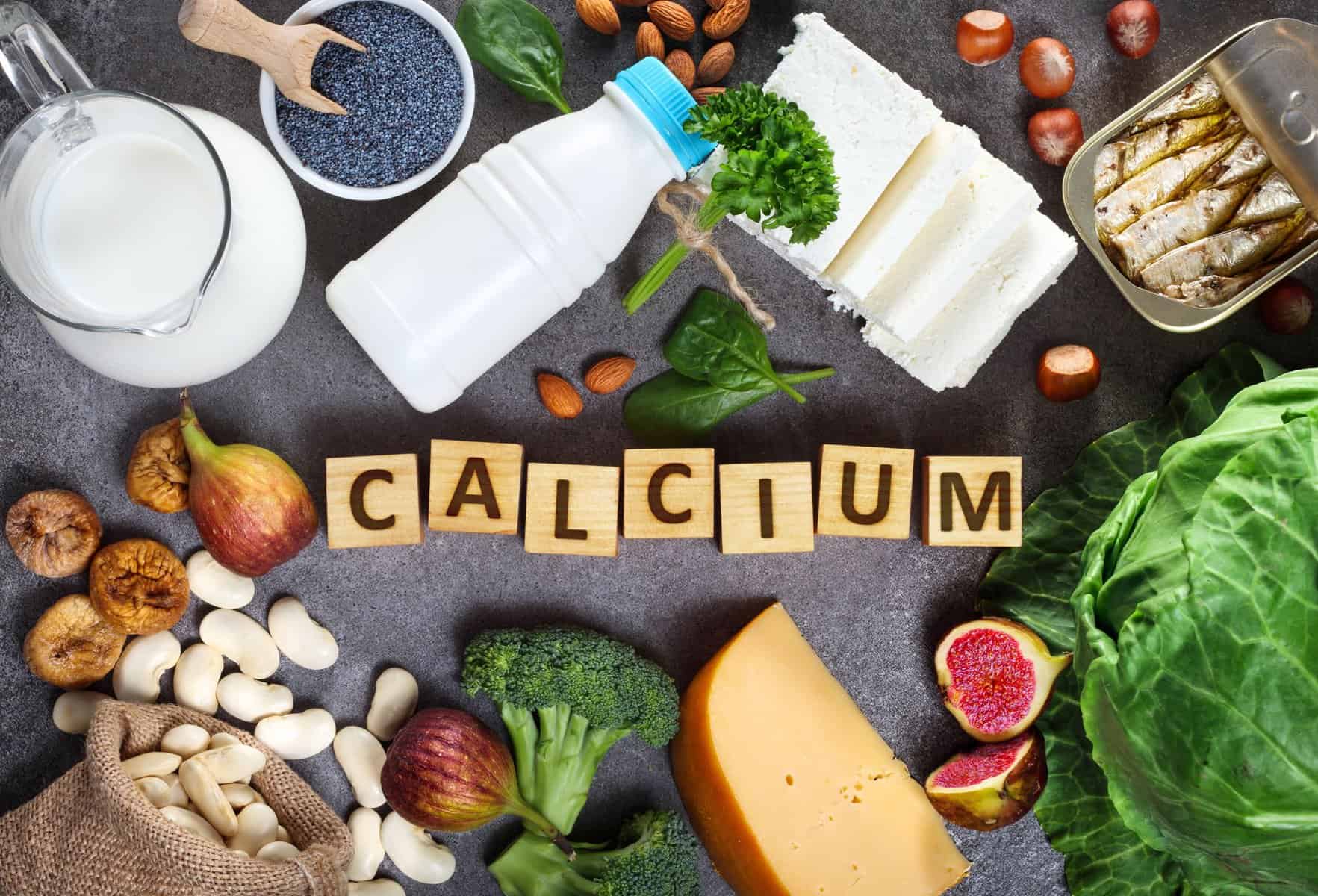
Sources of calcium & how to use them
Although many foods contain a small amount of calcium, it is recommended to regularly eat foods that contain a significant amount of calcium to meet your daily needs.
Dairy foods are a great source of calcium:
| Item | Suggested serve size | Amount of calcium (approximate) | Ways to use |
| Milk | 250ml (1 cup) | 300mg | · With cereal, muesli, or porridge
· In a smoothie · As a drink |
| Yoghurt | 200g (1 cup) | 350mg | · With cereal, muesli, or granola
· In a smoothie · With a curry (Greek yoghurt) |
| Cheese (cheddar/tasty) | 50g | 350mg | · In a toasted sandwich
· On pizza · On grainy crackers (e.g. Vita Weats) |
| Feta | 50g | 160mg | · In a salad
· In Spanakopita (Greek spinach & feta pie) · With egg & avocado on toast |
| Cottage cheese | 150g (3/4 cup) | 135mg | · In scrambled eggs
· In a smoothie · In muffins or mini frittatas |
| Ricotta | 120g (1/2 cup) | 200mg | · With banana on wholemeal crumpets or toast
· In cannelloni · With fresh fruit or in a fruit tart/galette |
| Kefir | 200g | 250mg | · As a drink |
If you aren’t keen on dairy, these foods also contain significant amounts of calcium:
| Item | Suggested serve size | Amount of calcium (approximate) | Ways to use |
| Soy milk
(check the nutrition info panel – choose non-dairy milks which contain more than 100mg calcium per 100ml) |
250ml (1 cup) | 300mg | · With cereal, muesli, or porridge
· In a smoothie |
| Soy yoghurt (calcium fortified) | 200g (1 cup) | 240mg | · With cereal, muesli, or granola
· In a smoothie |
| Tofu (calcium set) – check the ingredients list for calcium sulfate or 516 (a firming agent) | 150g | 300mg | · In a stir fry, soup, or curry
· Tofu scramble · In rice paper rolls · Crispy tofu burgers |
| John West Calcium+ tinned tuna
(contains tuna bone powder for calcium) |
90g (1 small tin) | 800-1050mg | · On crackers or rice cakes
· In a salad sandwich or wrap · With pasta |
| Sardines, tinned with small bones | 80g (1 tin) | 580mg | · On toast or grainy crackers
· With pasta · With a salad · In a salad sandwich |
Other sources of calcium include:
- Almonds: 20g (1 tbsp) provides about 50mg of calcium. This could be enjoyed as a snack or added to a salad.
- Chia seeds: 20g (1 tbsp) provides about 100mg of calcium. Chia seeds are a great addition to smoothies or used to make chia pudding.
- Milo: 20g of Milo powder provides 170mg of calcium. If you have Milo with 200ml milk, this will provide ~410mg of calcium!
- Up&Go: one 250ml serve provides 300mg of calcium.
Supplements: consult with your GP before taking a calcium supplement as it can interfere with certain medications, or it could put you at risk of excessive calcium intake.
If you have a nutrient deficiency or need assistance with other nutrition issues, make an appointment today for personalised advice from an experienced dietitian!
References:
- ABS (Australian Bureau of Statistics). Australian Health Survey: Usual Nutrient Intakes [Internet]. Canberra: ABS, 2015 [cited 2022 Sep. 20]. Available from: https://abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-usual-nutrient-intakes/latest-release#essential-minerals
- Australian Institute of Health and Welfare. Osteoporosis [Internet]. Canberra: Australian Institute of Health and Welfare, 2020 [cited 2022 Sep. 20]. Available from: https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoporosis
- Mountjoy M, Sundgot-Borgen J, Burke L, et al. The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S). British Journal of Sports Medicine 2014;48:491-497.
- National Health and Medical Research Council. Calcium [Internet]. Canberra: National Health and Medical Research Council, 2014 [cited 2022 Sep. 20]. Available from: https://www.nrv.gov.au/nutrients/calcium